If you were to create the perfect treatment session and treatment plan, what would you be sure to include? Would it include some patient education, exercise and a dash of manual therapy? Sure, arguably these may be important for every treatment plan, but do they all need to be in there? How about this - did the thought of showing empathy, encouragement and development of coping strategies come to mind? Often it is not the specific physical interventions which yield clinical outcomes, and instead, credit may be due to the soft skills: empathy, encouragement, and experiential learning. It may be true that doing less does mean more.
“Adversity - adverse or unfavorable fortune or fate; a condition marked by misfortune, calamity, or distress. ”
As physiotherapists, whether we realize it or not, some form of adversity is what typically brings patients knocking on our door. This adversity could take the form of a car accident, a sporting injury, a chronic disease or it could just be an insidious event. Most often, people see us when they can’t get past their adversity and return to a normal life. So what does this all mean in physiotherapy? Ever notice how two people can have similar injuries but very different levels of pain, disability and coping strategies? Or how one person can have a horrific injury and a great outcome, while another can have some minor event and a horrific outcome? Why is there such variety in people’s response to injuries?
Often there is a belief that there must be some underlying pathoanatomical cause for a person’s ongoing disability and pain. This may sometimes be the case, more recent research suggests that failure to overcome adversity is more often due to psychosocial factors. While we should still strive to rule out anatomical sources of pain, our assessment and treatment should include identifying any other factors that prevent recovery.
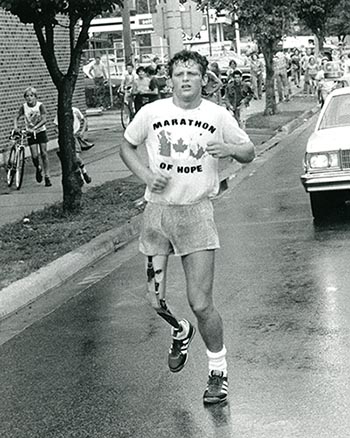 Now a few key points. Adversity in life is unavoidable and isn’t necessarily a bad thing; in fact, there is a body of literature suggesting that exposure to some adversity is associated with mental resilience, improved well-being, and less distress and disruption in the face of pain (ref). Even more important, adversity is something that can come to define us irrespective of whether we overcome our situation. Truthfully, we are enthralled and inspired by stories of individuals who face adversity. As a Canadian, the story that jumps to mind involves Terry Fox, a 21 year old man who lost his leg to cancer. Fox proceeded to embark on a run across Canada in 1980 to raise awareness and money for cancer, with the goal of raising one dollar from every Canadian. Fox would proceed to run a full marathon each day on a prosthetic that was not designed for running, literally one legged hopping each step of the way. He would go on to cover more than 5,000 km in his 143 day journey before being forced to quit when his cancer returned. He would pass away a year later, but his foundation has raised over 650 million dollars for cancer research since his death with annual memorial runs held in his honour to this day.
Now a few key points. Adversity in life is unavoidable and isn’t necessarily a bad thing; in fact, there is a body of literature suggesting that exposure to some adversity is associated with mental resilience, improved well-being, and less distress and disruption in the face of pain (ref). Even more important, adversity is something that can come to define us irrespective of whether we overcome our situation. Truthfully, we are enthralled and inspired by stories of individuals who face adversity. As a Canadian, the story that jumps to mind involves Terry Fox, a 21 year old man who lost his leg to cancer. Fox proceeded to embark on a run across Canada in 1980 to raise awareness and money for cancer, with the goal of raising one dollar from every Canadian. Fox would proceed to run a full marathon each day on a prosthetic that was not designed for running, literally one legged hopping each step of the way. He would go on to cover more than 5,000 km in his 143 day journey before being forced to quit when his cancer returned. He would pass away a year later, but his foundation has raised over 650 million dollars for cancer research since his death with annual memorial runs held in his honour to this day.
 Perhaps one of my favorite stories of adversity in sport is that of Derek Redmond, a 400 meter sprinter from the UK. Redmond ran a semi-final heat at the 1992 olympics and started off well but halfway through the race he pulled up and collapsed to the ground--torn hamstring. He eventually stood up after the rest of the field had finished the race and proceeded to hobble along the track, determined to finish the race. His father, who was watching in the stands, ran onto the field, pushing security out of the way, and helped his son finish the race to a standing ovation of 65,000 people. Take the time to watch the video - my apologies for the sappy music, this story doesn’t need it!
Perhaps one of my favorite stories of adversity in sport is that of Derek Redmond, a 400 meter sprinter from the UK. Redmond ran a semi-final heat at the 1992 olympics and started off well but halfway through the race he pulled up and collapsed to the ground--torn hamstring. He eventually stood up after the rest of the field had finished the race and proceeded to hobble along the track, determined to finish the race. His father, who was watching in the stands, ran onto the field, pushing security out of the way, and helped his son finish the race to a standing ovation of 65,000 people. Take the time to watch the video - my apologies for the sappy music, this story doesn’t need it!
“Perseverance: steadfastness in doing something despite difficulty or delay in achieving success.”
The interesting thing about these stories of adversity is that both Fox and Redmond did not accomplish what they originally set out to do. What they did do was demonstrate incredible perseverance and they're now recognized not for what they accomplished but how they stood up to adversity. So how do stories like these relate to our work as healthcare providers?
Daily, we see people experiencing adversity and we should always be honoured that they are willing to entrust us to assist them through this process. We should also realize what a massive impact we can have in empowering and educating these patients. Quite often, patients will see their situation as an insurmountable obstacle that they are unable to overcome. As much as our job is to build their physical resilience, perhaps more important is our guidance inspiring mental resilience or grit. And sometimes, it isn’t about doing something different but reframing the situation that leads to success. I remember hearing Rick Hansen speak at a medical conference a decade ago. For those of you not familiar with his story, Rick was a friend of Terry Fox who was inspired by Fox’s efforts and set out to push his wheelchair around the world. He got a rousing send off in Vancouver but within a few days, found himself alone on the road in wet and cold conditions. Hansen had developed severe tendonitis and came back to the bus saying there was no way he could continue. His coach asked him if he could go out and do one more push of his wheelchair - Hansen said of course. The coach then asked him for one more and then ten more and then a hundred more and eventually wheeled himself over 40,000 kilometers, averaging 30,000 strokes a day. Needless to say, Hansen might not have met his goal if he hadn’t broken it down and took it one push at a time. Does this story sound like something healthcare worker’s do or could do?
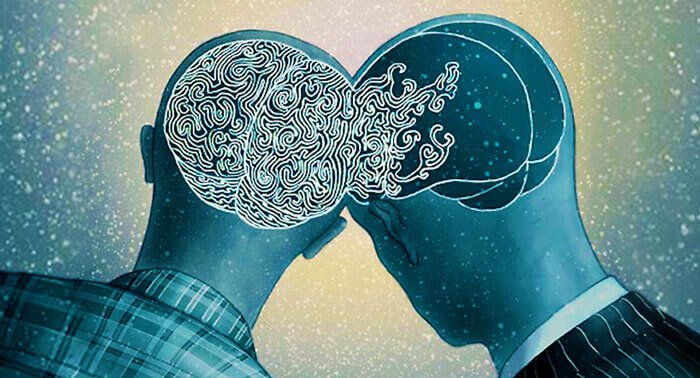
“Empathy: The experience of understanding another person’s condition from their perspective. You place yourself in their shoes and feel what they are feeling.”
 So what can we do to help? As PTs, our role is to educate, empower and collaborate with our patient’s to develop or refine their current coping strategy. But first, everything starts with our ability to listen and validate the unique story each patient has to tell. This is an important component of empathy and there is mounting evidence that this is both a critical component of the therapeutic relationship and leads to improved clinical outcomes. Studies have estimated that up to 50% of patients feel that their physician did not care for them (ref) despite there being significant evidence that empathy can influence clinical adherence and effectiveness (ref). What makes the lack of empathy even more puzzling is that it is a skill that can be taught. In one trial, physicians were given three three hours of training in empathy and were rated two months later as being more empathetic by patients (ref).
So what can we do to help? As PTs, our role is to educate, empower and collaborate with our patient’s to develop or refine their current coping strategy. But first, everything starts with our ability to listen and validate the unique story each patient has to tell. This is an important component of empathy and there is mounting evidence that this is both a critical component of the therapeutic relationship and leads to improved clinical outcomes. Studies have estimated that up to 50% of patients feel that their physician did not care for them (ref) despite there being significant evidence that empathy can influence clinical adherence and effectiveness (ref). What makes the lack of empathy even more puzzling is that it is a skill that can be taught. In one trial, physicians were given three three hours of training in empathy and were rated two months later as being more empathetic by patients (ref).
Once we understand the patient’s story, we can start developing skills and tools the patient can use to persevere and thrive. Often patients are worried and unsure why their pain exists and for physiotherapists this creates an opportunity to build mental resilience. Sounds good right, but how we do that? Let’s start by helping patients reconceptualize the problem and understand pain. Give a brief explanation that “hurt does not always equal harm” and if appropriate, describe how current understandings of pain can be influenced within the biopsychosocial framework. Once your patient begins to understand their symptoms as a tissue sensitivity rather than tissue damage, patient self-efficacy can be boosted by providing some basic active coping strategies. This may come in the form of simple pacing strategies, temporary movement modifications or simple exercises to gradually expose and encourage patients to confront and challenge their symptoms. Reassure and get patients to flirt with the boundary of their symptoms so they start to find comfort around their discomfort. Each patient that is experiencing adversity will have different challenges cognitively, emotionally and physically, so it will be up to us to help determine how we can start to assist with overcoming them. Finally, celebrate your patients successes and help them back up (Hopefully just figuratively!) when they stumble. Rehabilitation is a process and it is almost never without its ups and downs.
 We must remember that humans are active learners across the lifespan and should be encouraged to embrace their innate curiosity and explore and interact with their symptoms. It is through this experiential learning, especially in the face of adversity, where memories form and adaptation occurs. Often the skills learned in adverse situations can transfer over to many aspects of our lives and improve our relationships, work and education. So can we do better to in our approach when helping patients overcome their adversity? Is it always necessary to intervene with specific intervention or is active listening, validation, thoughtful questioning and encouragement sometimes the most valuable intervention? Just like Terry Fox, Derek Redmond and Rick Hansen, patients can learn to reframe and overcome significant adversity if we create a caring and supportive environment.
We must remember that humans are active learners across the lifespan and should be encouraged to embrace their innate curiosity and explore and interact with their symptoms. It is through this experiential learning, especially in the face of adversity, where memories form and adaptation occurs. Often the skills learned in adverse situations can transfer over to many aspects of our lives and improve our relationships, work and education. So can we do better to in our approach when helping patients overcome their adversity? Is it always necessary to intervene with specific intervention or is active listening, validation, thoughtful questioning and encouragement sometimes the most valuable intervention? Just like Terry Fox, Derek Redmond and Rick Hansen, patients can learn to reframe and overcome significant adversity if we create a caring and supportive environment.
AMP’d Clinical Bottom Line
-
Listen, be empathetic, and validate your patient’s experience.
-
Recognize coping strategies may differ from patient to patient.
-
Identify and develop strategies which encourage the patient to explore the nature of their symptoms, foster active learning and acquire the skills necessary to overcome their adversity.


STEVE YOUNG, BSCPT, BA SEAN OVERIN, BHK, MPT









