Having worked in a chronic pain program for several years early in my career, I will fully disclose my bias toward the pain sciences. In many situations it has served me well, but there have been times I have used it to explain too much. Differently said, I may have tried to “ram” pain science down the “throat” of pain-processing-innocents, possibly alienating them in the process. With that in mind this blog starts to address how to move toward a middle ground, regardless of your “tissue issue” or “pain science” bias, to best help our clients.
Nijs and colleagues (ref) published a beautiful paper intended to help manual therapists identify central sensitization (CS) in clients. It is fair to say that pain science directed education and interventions are likely best suited for clients with CS largely in part because you can’t touch them (allodynia and wind-up phenomenon to manual therapy) and they are scared to move or exercise (fear avoidance and beliefs that movement will harm them). So, really, where else are you going to start with them?
Nijs (ref) makes an argument for this in the rehabilitation of chronic spinal pain, stating that intensive early pain science education will pay off as rehabilitation is moved into motor control exercise using a time contingent approach to exercise, rather than a symptom based approach. A study in progress by Dolphens (ref) aims to compare pain, disability and brain cortical changes between traditional physical therapy approach (i.e. pathoanatomical reasoning, education, and motor control exercise), control group and this proposed “modern neuroscience approach,” (results are pending). However, enough evidence exists for pain neuroscience education for Louw and colleagues (ref) to conduct a review and conclude that there is, “compelling evidence that NE may be effective in reducing pain, increasing function, addressing catastrophization, and improving movement in chronic MSK pain.”
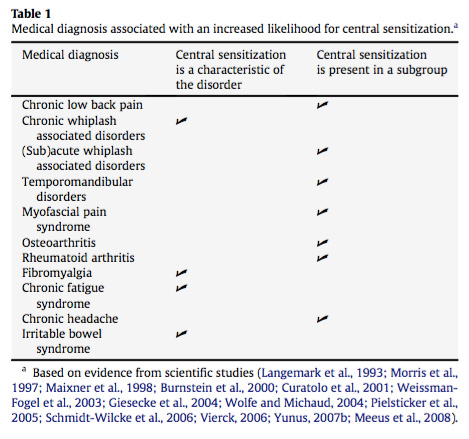
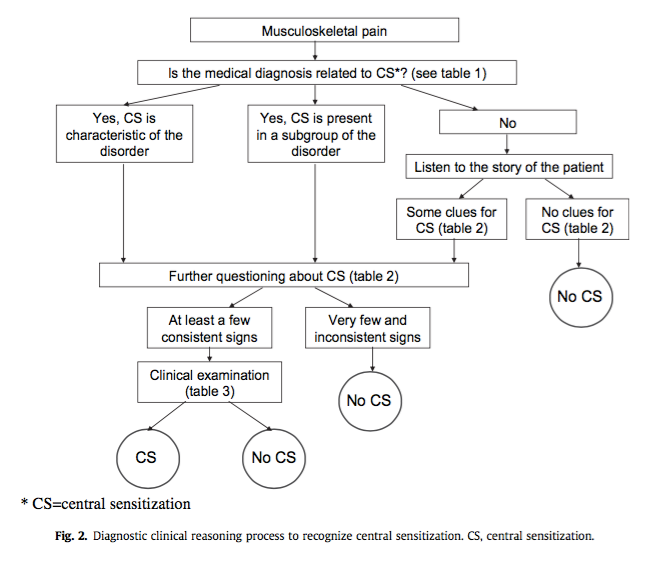
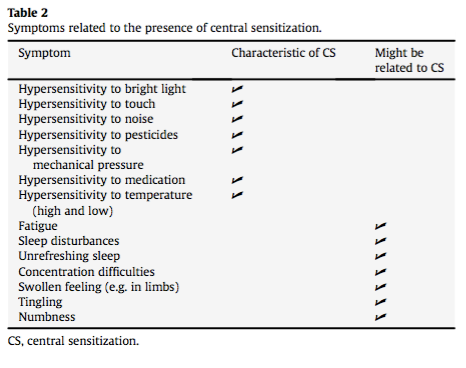
In their paper Nijs and colleagues present a basic algorithm to help guide our clinical reasoning (see figure 2). I emphasize guide, because we all know our clients' presentations rarely fit into tidy boxes or models of treatment. Thus, Nijs suggests to simply be aware of conditions in which the literature supports CS as part of the presentation, and those conditions in which CS is known to exist in a subset of the population (see table 1). They go on to suggest screening for factors in the history (see table 2) and assessment (see table 2) that are consistent with a CS presentation.
While I fully endorse the quick and easy subjective screening, using all the physical assessments they suggest is simply not feasible. Arguably, the best and most efficient tests to incorporate into clinical practice would be: (1) manual palpation for pain pressure threshold (PPT) remote to area of primary pain (e.g. side to side comparison), (2) joint end feel (increased sensitivity to muscle and joint end feel testing), (3) bilateral heightened sensitivity to ULTT1 (Bilateral loss of >30 deg elbow extension), and assessment of PPT pre to post exercise (i.e. bike test at 10-20 Watts for 2-4 min; expect PPT to increase if CS not present).
As for acute tissue related injury, we all know how to screen and assess for this, as we spent two plus years in school being told what these presentations look like (but it is never as clear cut as it is in the text books… more on that in a future blog: “Fast responders and the sensitized pain system: There is a role for pain education outside of central sensitization”). But for a quick review, let us consider the most obvious factors that represent acute injury. First, history always takes precedent; physical assessment is used to confirm or refute your hypothesis. Factors suggesting acute injury include:
-
Distinct or classic mechanism of injury (MOI) (such as the knee valgus and rotation in a non-contact ACL injury).
-
Findings consistent with tissue healing time frame (i.e. within 10 weeks and steady improvement; if it is longer than this start thinking about nervous system sensitivity as opposed to a poor healing response).
-
Obvious clinical tissue signs → more than just one of the cardinal signs of inflammation (I would say at least 2 out the following 3 should be present: redness, swelling and or heat; pain and loss of function are an obvious given), as well as hematoma/bruise/ecchymosis
So this Nijs paper in combination with our past training will provide us with some idea on how to screen for CS and acute tissue injury in our clients. However, what happens when these two things interact?
A recent case had me consider this question. A patient came in with shoulder pain after a traction MOI at work 1 week prior, and a history of a similar incident for the right shoulder many years ago which lead to a protracted return to work for right shoulder pain and/or injury (by now I hope we can agree that pain and injury are not always related). During the physical exam, the client demonstrated pain and limited range of motion in all directions. Obviously this made the gathering of any meaningful data with various tests impossible (however, read this blog which questions how special shoulder special tests really are). Further, the patient also demonstrated fear-avoidant behaviour, allodynia locally over the involved anterior shoulder only, and contralateral ULTT1 was unremarkable. Thus far, I am thinking there is a clear and distinct MOI that suggests acute injury, but a history that may contribute to a sensitized nervous system, and a physical exam that was limited due to pain. This had me thinking that the nervous system might be over protecting the left shoulder, as the patient’s pain and limited function seemed to be out of proportion to their reports of being able to work for a few hours after the MOI.

We started discussing some pain science early on, in conjunction with regional manual therapy and exercise as tolerated, but the patient did not feel the pain science education applied to this situation. I pursued for a few more sessions, with no real engagement or “buy-in” to this approach at which point I decided to stop forcing the issue. When we stopped formal pain education, the client started to improve.
A recent qualitative study by Robinson and colleagues (ref) evaluated themes present in 10 individuals with persistent pain after a single group pain neuroscience education session. These authors found that most people found the session a positive and personally relevant experience (8 of 10) with some participants demonstrating a reconceptualizing of their pain. Two of 10 participants reported that they did not find the content relevant to their condition as they had tried the strategies previously without success or didn’t understand the content. These authors highlighted the clinical relevance of making pain science education relevant to the individual and how pain neuroscience interacts with their condition. This theme was also discussed in a great podcast (listen here) where Cory Blickenstaff and Erik Meira discuss their general approach to interweaving pain neuroscience education into their treatment. They suggest the need to find the point in the client’s narrative (i.e. the story they tell themselves about why they are in pain) that assists you in making pain science education relevant to them. Cory describes setting up a clinical experiment that confronts the client’s narrative which challenges their beliefs about their pain. This is a feature of exposure therapy, which aims to disconfirm a thought virus or some belief that a task or movement is harmful.
So what is the take home? Clinicians can leverage contemporary pain science reasoning to guide our clinical decision-making when a presentation does not “add up” or make sense and use education interventions when the client is ready for pain science education. But keep a watchful eye for your regular signs of acute injury despite a history of suggesting a sensitized nervous system and use a test-retest approach for all your interventions including education. If your patient is not responding to a treatment modality, we need to stop and reflect on what we could change. Let’s focus on the things that help our patients move forward.
In the above case, I continued to let pain science help guide my clinical reasoning with exposure based exercises, pacing strategies, and lots of encouragement. I decided not to force formal pain science education on the client, and kept up suspicion that there may be a tissue injury involved. To be honest, tissue issues and pain science reasoning most likely exist on a continuum, where clinicians must appreciate that different clients can present with a different mixture of each.
A Pain Science approach helps us side step fear, and optimize beliefs about the body as a resilient and strong entity. Tissue-Issue reasoning prompts us to respect tissue healing times, and optimize activities and behaviour to idealize a physiologic healing process. As physiotherapists, a priority is to help people feel empowered to move. Giving patients appropriate education on their condition likely is our best intervention! Let us not taint this education with fear of tissue damage when it is not appropriate; rather, ensure your patients understand how amazing, strong, and resilient their body is even when it hurts.
Clinical bottom line:
-
Watch out for obvious signs of acute injury, but know that a large majority of pain presentations are not simply a result of “faulty” tissues.
-
Be aware of signs of central sensitization using the Nijs paper as a guide. People with these presentations benefit greatly from pain neuroscience education and explanations that pain is not only a representation of tissue injury.
-
Use your most powerful tool and educate clients appropriately to understand that their bodies are capable and resilient structures! People respond to positive messaging.

Author: CURTIS TAIT, BSC, MPT, IMS









